- For Providers
- For Brokers
Individuals & Families
- Global Individual Health
- Spanish Domestic Individuals
Employers
- SME Employer Health
- Large Corporation Health
- Spanish Domestic Employers
IGO/NGO
- IGO/NGO Health
Individuals & Families
Top Destinations We Cover
Expat Health Insurance
- Inside Expat Health Hub
- Retiree guide to International health Insurance
- A guide to International health Insurance for working abroad
- Expat Health Insurance Explained
- Student guide to International health Insurance
- Moving abroad while pregnant
Choosing Health Insurance
- Travel Insurance vs International Health Insurance
- Choosing Health Insurance
Country Guides
- Country Guides
FAQ
- Frequently Asked Questions
Employers
Global Health Benefits Europe
- Employers Health Plans
- Cigna Inspire Plan
2 - 149 Employees
- International Health Plans
Large Corporates
- Corporate Health Plans
Global Health Benefits North America
- Employers
- OCONUS
- Students and Faculty
- Government
Clinical
Member resources
- Useful Documents & Information
- U.S Prescription Drug List
Client
- Employer Log In
IGO/NGO & Government
Government Officials
- Government Officials
Client
- Employer Log In
Topics
Individuals & Families
-
Types of Cover
-
Where We Cover
-
Resources
- Inside Expat Health Hub
- Retiree guide to International health Insurance
- A guide to International health Insurance for working abroad
- Expat Health Insurance Explained
- Student guide to International health Insurance
- Moving abroad while pregnant
- Travel Insurance vs International Health Insurance
- Choosing Health Insurance
- Country Guides
- Frequently Asked Questions
-
For Members
Employers
-
Our Plans
-
Clinical
-
For Members
IGO/NGO & Government
Health Blog
For Brokers
Virtual health: The answer to a challenging healthcare landscape
Virtual health: The answer to a challenging healthcare landscape
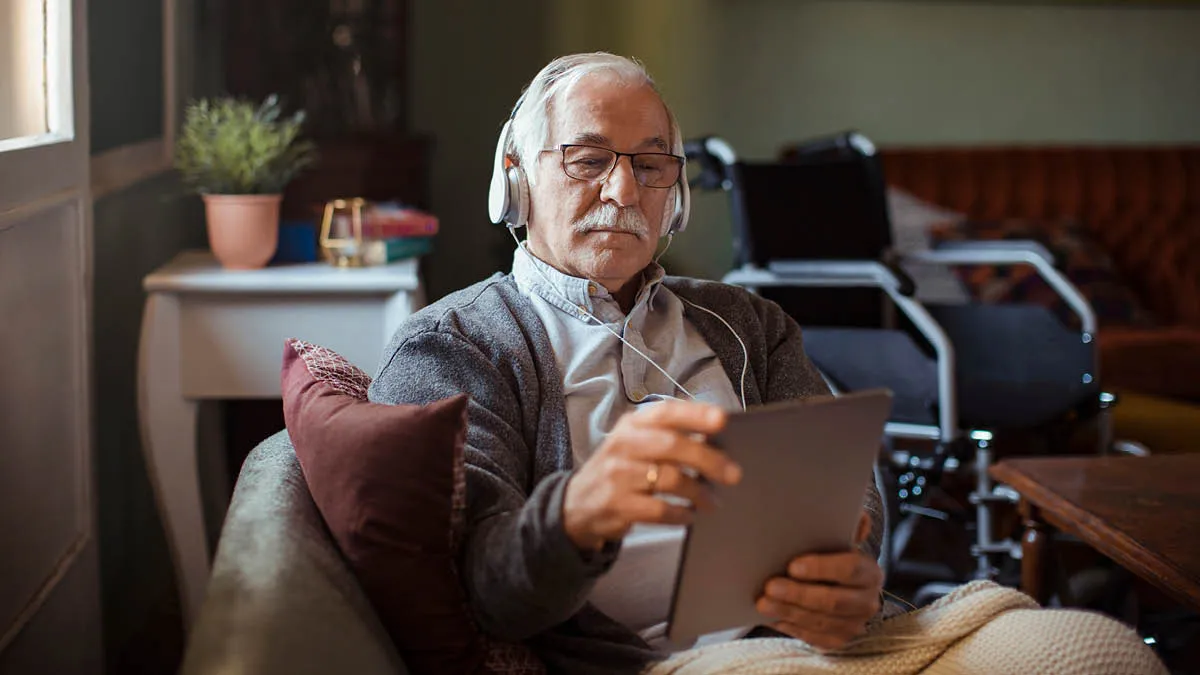
Record inflation, workforce shortages and rising levels of chronic disease are fueling a major transformation in healthcare, with new technologies, diagnostic tools and data changing how, where and when it can be delivered. Cigna Healthcare is at the forefront of this, constantly seeking new technologies to improve patient services and outcomes as virtual modes of care enter the mainstream of clinical practice.
Traditional notions of ‘seeing the doctor’ are changing. Over the last two years, four in 10 people have consulted a doctor over the phone or virtually and more than 40% now consider it as good as in-person consultations.
A combination of record inflation and increased use of health services, both of which emerged out of the Covid-19 pandemic, is fueling significant increases in medical costs. Global healthcare spending rose by more than 40% between 2018 and 2022, reaching US$12 trillion[1], and the cost of delivering individual care continues to escalate[2].
The cost of living is impacting human well-being and vice versa in a vicious cycle. Cigna Healthcare’s latest 360 Global Well-Being Survey (360 survey), conducted in early 2023, found six in 10 (63%) respondents around the world feel their ability to meet their or their family’s medical needs is only “fair” or “poor”. Virtual health could be the key to enabling people to meet their medical needs at lower cost and with greater convenience.
Meanwhile, with governments struggling to meet the rising needs of their populations and facing an alarming shortage of healthcare workers[3], there is a growing acceptance by the industry and consumers that the way forward for healthcare is through rapid innovation.
Overcoming the barriers of access to care
Access to care is the most persistent challenge facing health systems globally[1], with long waiting times for health services in many countries, especially those with public systems. In the UK, for example, the waiting list for hospital treatment hit a record of 7.2 million patients in January 2023. In December 2022, half of all UK hospital A&E patients had to wait more than four hours to get treatment, a record high for the country[2].
Our 360 survey found that 40% of respondents have struggled to get an appointment with a doctor quickly when they were sick in the last two years. This is a huge cause for concern, because the ability to seek timely medical attention can mean the difference between life and death in some cases.
The previous edition of our 360 survey conducted in 2022 found that not being able to get an appointment with a healthcare professional was the main reason for delayed investigation of health issues for one out of five (21%) respondents who experienced such a delay. Interestingly, 22% of those respondents told us they ended up turning to virtual health to seek the medical advice they needed.
Amid the many barriers to care, however, virtual health has firmly established its position as an alleviating and potentially life-saving innovation[3]. It improves operational efficiency across primary and tertiary settings, optimizes appointment schedules, and eliminates patients’ travel time. With 95% of the world’s population now covered by a mobile broadband network[4], telehealth has now become a permanent fixture of system delivery[5].
But virtual health is more than telehealth; it encompasses a much wider breadth of clinical practice, including remote patient monitoring, imaging and diagnostics, virtual triage and hospital management, patient data and more recently, artificial intelligence (AI) which offers enormous potential to further reduce costs, improve efficiency and enhance patient outcomes.
Traditional notions of ‘seeing the doctor’ are changing. Over the last two years, four in 10 people have consulted a doctor over the phone or virtually and more than 40% now consider it as good as in-person consultations.
A combination of record inflation and increased use of health services, both of which emerged out of the Covid-19 pandemic, is fueling significant increases in medical costs. Global healthcare spending rose by more than 40% between 2018 and 2022, reaching US$12 trillion[1], and the cost of delivering individual care continues to escalate[2].
The cost of living is impacting human well-being and vice versa in a vicious cycle. Cigna Healthcare’s latest 360 Global Well-Being Survey (360 survey), conducted in early 2023, found six in 10 (63%) respondents around the world feel their ability to meet their or their family’s medical needs is only “fair” or “poor”. Virtual health could be the key to enabling people to meet their medical needs at lower cost and with greater convenience.
Meanwhile, with governments struggling to meet the rising needs of their populations and facing an alarming shortage of healthcare workers[3], there is a growing acceptance by the industry and consumers that the way forward for healthcare is through rapid innovation.
Overcoming the barriers of access to care
Access to care is the most persistent challenge facing health systems globally[4], with long waiting times for health services in many countries, especially those with public systems. In the UK, for example, the waiting list for hospital treatment hit a record of 7.2 million patients in January 2023. In December 2022, half of all UK hospital A&E patients had to wait more than four hours to get treatment, a record high for the country[5].
Our 360 survey found that 40% of respondents have struggled to get an appointment with a doctor quickly when they were sick in the last two years. This is a huge cause for concern, because the ability to seek timely medical attention can mean the difference between life and death in some cases.
The previous edition of our 360 survey conducted in 2022 found that not being able to get an appointment with a healthcare professional was the main reason for delayed investigation of health issues for one out of five (21%) respondents who experienced such a delay. Interestingly, 22% of those respondents told us they ended up turning to virtual health to seek the medical advice they needed.
Amid the many barriers to care, however, virtual health has firmly established its position as an alleviating and potentially life-saving innovation[6]. It improves operational efficiency across primary and tertiary settings, optimizes appointment schedules, and eliminates patients’ travel time. With 95% of the world’s population now covered by a mobile broadband network[7], telehealth has now become a permanent fixture of system delivery[8].
But virtual health is more than telehealth; it encompasses a much wider breadth of clinical practice, including remote patient monitoring, imaging and diagnostics, virtual triage and hospital management, patient data and more recently, artificial intelligence (AI) which offers enormous potential to further reduce costs, improve efficiency and enhance patient outcomes.
Familiar AI applications include virtual assistants – which can provide round-the-clock guidance on how to access health services, and the use of AI in summarizing and extracting key information from medical records. AI can also help enhance the effectiveness of remote patient monitoring by analyzing data from monitoring devices and providing real-time insights and alerts to enable healthcare providers to quickly address any problems[9]. While attention must be paid to the proper and ethical use of AI to manage bias, security, and other issues, it nevertheless offers a tremendous range of benefits and new possibilities.
Enhancing health equity
“Gaps in access to care are affecting the well-being of people around the world. It is also one of the contributing factors to health disparities arising from differences in socioeconomic status, geographical location, and physical disabilities. By delivering health services virtually to people when and where they need them, we are closing the gaps in healthcare access and giving everyone a fairer chance at staying healthy.”
– Jason Sadler, President, International Health, Cigna Healthcare
Link between coordination and affordability
Virtual health has great potential to bring access and affordability – two key pillars in the drive to achieve healthcare equity[10]. But there are still hurdles to overcome in terms of managing complex conditions effectively and remotely.
Research has found that virtual healthcare can also reduce health system costs by offering more timely care, thus mitigating the need for expensive procedural or specialist follow-up. At the same time, patients, and clinicians have less need to travel to consultations – thus lowering health system costs when these trips are system-funded[11]. Furthermore, virtual health is more affordable overall than in-person care. For instance, a study of patients with cardiovascular disease in the US found that the mean telehealth cost per person was US$112.8, while for in‐person outpatient encounters it was US$161.4.
Coordinated care is the next evolution in the virtual health journey. Working in unison, telehealth, patient monitoring, and data interoperability are allowing teams of healthcare professionals and relevant agencies to manage chronic conditions away from the hospital. This ultimately reduces hospital visits, improves outcomes and lowers the economic burden of care on already struggling systems. Such innovations are driving new behaviors, routines, and ways of working in all clinical settings, driving administrative efficiency, cost-effectiveness and a better user experience for patients and clinicians alike.[12]

Virtual case management
Cigna Healthcare already supports its customers with a range of virtual health services, including virtual case management and remote consultations. Virtual case management is a service where a clinician – normally a nurse, but sometimes a doctor – is appointed as the customer’s contact person to help handle their care and guide their overall health journey. This is particularly useful for people suffering from complex or sensitive conditions which make them more vulnerable or mean they need added support. The company also serves many globally mobile individuals, for whom virtual consultations are a great solution. They can talk to their primary care physician remotely whenever they need to, and can ensure consistent follow-up, wherever they are in the world, with the same physician each time.
Mental health support
We were an early advocate of virtual health, offering tools and services via our popular Wellbeing® app back in the pre-COVID days. Today, we offer comprehensive digital solutions through our joint ventures, NAS Neuron in the Middle East and Honeysuckle Health in Australia, and in partnership with providers like Teladoc Health, a global leader in whole-person virtual care. As part of these solutions, we see a great case for the use of virtual health to address mental health issues. Whether through self-guided activities delivered through an app, or one-on-one live coaching sessions, virtual mental health services remove barriers and stigma to empower people to get the care they need and ensure early intervention for mental health problems[13].
Balancing act: virtual health as a viable alternative to in-person care
The rapid rise of virtual care in clinical and patient settings is fueling a new debate over how to right-site care, i.e., which mode is best suited to which scenario. Healthcare providers are already experiencing a sea change in how they administer care amid the rise of data science, mobile networks, and biosensors, along with the growing popularity of telemedicine and remote patient monitoring. A 2022 study revealed that 63% of clinicians anticipate conducting most consultations remotely over the next 10 years, while 49% believe that patients will receive most of their care at home in the next decade[14].
But change is not happening as fast everywhere. In Australia, for example, a recent survey of 248 clinical staff from 20 communities across the country’s most remote regions found that while telehealth can improve access, significant questions are still being worked through about how, when, and to what extent it should be used. While staff shortages are impacting health systems across the globe, proper training and guidelines around digital infrastructure can ensure that care is appropriately sited across communities[15].
On the patient side, our latest 360 survey found that people are becoming increasingly familiar with at least some elements of virtual health; an average of four in 10 respondents had communicated with doctors by telephone or virtually for general health consultations (see Appendix for activities done by respondents through virtual health channels in different markets). Overall, more than four in 10 of our survey respondents expressed this satisfaction, including with regard to ease of arranging consultations (46%), general convenience (42%), being listened to and understood (46%), being given the right amount of time and attention (45%), and follow-up care (50%).
There are also variations in uptake and perception based on demographics, especially in terms of age groups. The 360 survey found the younger generation has more experience with virtual health: 16-24 year-olds had used it most, with 45% having consulted a doctor over the phone or virtually, closely followed by the 25-34 (44%) and 35-49 (43%) age brackets. But younger age groups are usually less reliant on health systems, so it is important to encourage greater usage and deliver targeted health promotion activities towards age groups over-45, of which only 35% to 38% say they have previously consulted a doctor over the phone or virtually.
Virtual or in-person?
“It’s not a case of choosing one or the other. Both play their part in the patient journey. We will never have a completely virtual health system – nor do we want one, as it just wouldn’t be effective. However, clinicians realize that virtual health offers an opportunity to improve access and provide care outside the four walls of their medical practice.”
– Dr. Stella George, Chief Medical Officer, International Health, Cigna Healthcare

Continuous improvement and innovation drive virtual health adoption
As virtual health becomes a more normalized option for patients, healthcare service providers have a responsibility to help build trust with patients and optimize their care experience. This can be achieved through better understanding of the needs of patients and barriers to adoption, and more dedicated training for clinicians looking after patients through virtual channels.
As technology continues to advance, we believe the quality of virtual health will keep improving. At Cigna Healthcare, we’ve been investing in digital and analytics capabilities to enhance our health services. The integration of virtual health and data analytics enables us to capture and leverage large amounts of data to produce intelligent insights into the needs of our customers, allowing us to serve them more effectively. For example, Honeysuckle Health’s Injury Support Program, a telephone service which provides clinical and care coordination support to help customers who have suffered a workplace injury with their recovery, deploys analytics to provide targeted support to those who will benefit most from the program.
Beyond reducing costs and improving access to healthcare, virtual health is bringing us a step closer to a truly patient-centric healthcare system, where we can offer people the most suitable care whenever and wherever they need it. We are undoubtedly living through a challenging moment for health systems around the world, but the widespread adoption of virtual health may well ease our transition into a new and more effective mode of healthcare. You can download this report easily as a PDF:
1 https://www3.weforum.org/docs/WEF_Global_Health_and_Healthcare_Strategic_Outlook_2023.pdf
2 https://www.wtwco.com/en-us/insights/2022/10/2023-global-medical-trends-survey-report
3 https://www3.weforum.org/docs/WEF_Global_Health_and_Healthcare_Strategic_Outlook_2023.pdf
4 https://www.weforum.org/agenda/2022/11/global-healthcare-mental-health-survey/
5 https://commonslibrary.parliament.uk/research-briefings/cbp-7281/
6 https://www.progressivepolicy.org/wp-content/uploads/2021/11/Telehealth-Saves-Money-and-Lives-Lessons-from-the-COVID-19-Pandemic-PPI-AFP.pdf
7 https://www.gsma.com/r/somic/
8 https://www.nature.com/articles/s41591-021-01447-x
9 https://www.forbes.com/sites/bernardmarr/2023/03/02/revolutionizing-healthcare-the-top-14-uses-of-chatgpt-in-medicine-and-wellness/?sh=42341a876e54
10 https://www.weforum.org/agenda/2023/01/telemedicine-global-health-equity-at-home-davos23/
11 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7605980/
12 https://nursing.jmir.org/2020/1/e20282/
13 https://www.teladochealth.com/organizations/health-plans/mental-health
14 https://www.weforum.org/agenda/2023/01/telemedicine-global-health-equity-at-home-davos23/
15 https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-09265-2
Related articles
@Cigna 2025
This article serves only as a reference and is intended for informational purposes only. Nothing in this article constitutes legal, tax, financial planning, health or medical advice including diagnosis or treatment. Any reference to products or services offered by Cigna are available except where prohibited by applicable law and subject to terms and conditions. Cigna have no involvement in, nor are we liable for, any decisions and/or outcomes that are made or determined by FocusPoint International.
Contact Us
Whether you wish to speak to our sales team or get general help if you are already a Cigna Healthcare® member, we’ll get you to the right information.
Contact InformationPopular Links
Resources
© Cigna Healthcare. All rights reserved.
*Please note, this is a representation of the benefits available and does not contain the terms, conditions, and exclusions specific to each benefit. The benefits may be subject to change. Some benefits may be part of an optional module. Please see the Customer Guide for full details.
This website is provided by Cigna European Services (UK) Limited, a company incorporated in England and Wales having its registered address at 13th Floor, 5 Aldermanbury Square, London EC2V 7HR and registered number 00199739. The Cigna Healthcare name, logo and other Cigna Healthcare marks are owned by Cigna Intellectual Property, Inc., licensed for use by The Cigna Group and its operating subsidiaries.
Our Policies are underwritten by Cigna Global Insurance Company Limited, a private limited company under Guernsey Law, with registered address office at PO Box 155, Mill Court, La Charroterie, St Peter Port, Guernsey, GY1 4ET, and company number 41925. Cigna Global Insurance Company Limited is authorised and regulated by the Guernsey Financial Services Commission for the conduct of insurance business in Guernsey.
This communication is being issued and/or distributed by Cigna Insurance Management Services (DIFC) Limited which is regulated by the Dubai Financial Services Authority.
Selecting these links will take you away from Cignaglobal.com. Cigna Healthcare does not control the linked sites' content or links.

